
Degenerative Joint Disease
Blood testing can help identify degenerative joint diseases and allow management to start sooner than waiting for clinical presentation.
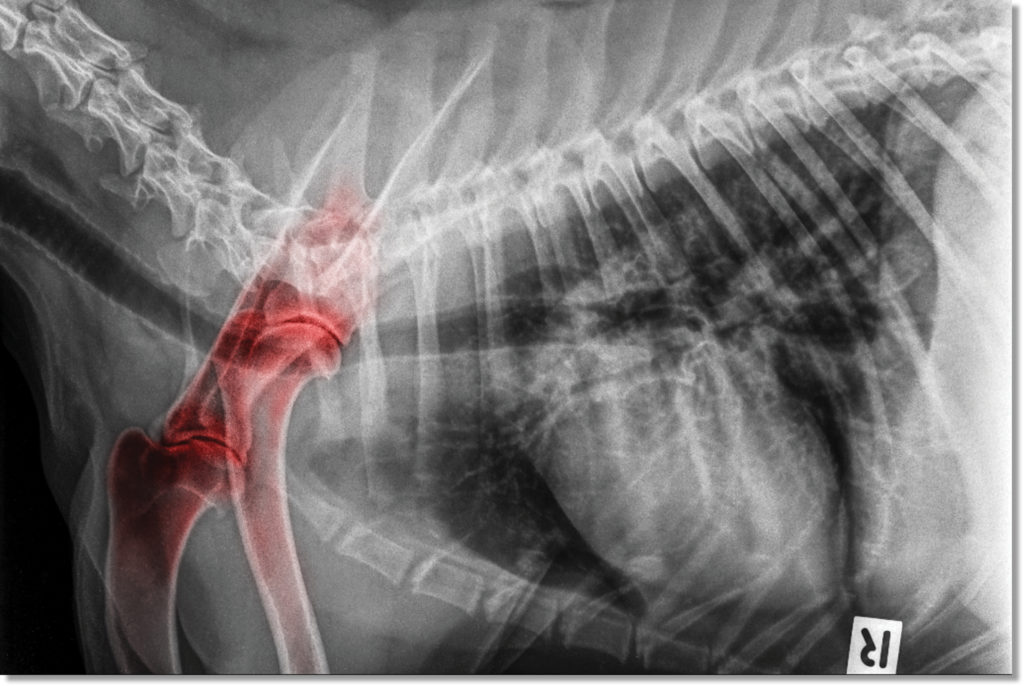
Degenerative joint disease (DJD) is a common, age-related breakdown of the joint. Other risk factors include weight, breed, genetic line, and diet. Osteoarthritis (OA) is the most commonly diagnosed DJD in both human and veterinary medicine and affects 20% of dogs older than one year and a stunning 80% in dogs greater than 8 years . Certain breeds are predisposed to OA with males having a higher incidence than females, especially in neutered animals. Other DJD include intervertebral disk disease (IVDD), degenerative myelopathy (DM), and immune mediated polyarthritis (IMPA). Sooner or later, many pets succumb to the crippling effects of DJD with most not being clinically diagnosed until it reaches an advanced stage and clinical signs are obvious.
Hyaluronic Acid: Blood Test for DJD
Serum hyaluronic acid (sHA) is a blood test for the early detection of degenerative joint disease (DJD) as well as post-therapeutic monitoring for therapy effectiveness. Positive sHA values are to be interpreted as positive for DJD provided the patient does not have severe liver disease. The use of CRP (dogs) or HPT (cats) assists in the severity of osteoarthritis, treatment efficacy, and the differential diagnosis of IMPA. Patients using HA containing supplements should be taken off supplements 48 hours prior to blood draw to prevent interference.
Common Applications
- Patients over 5 years old (screening)
- Large & giant breed dogs
- Patients with early signs of joint pain
- Patients susceptible to DJD/OA
- Injury to joint(s)
- Active/working/sporting dogs
- Breeds predisposed to joint and skeletal disorders
- Patients with known DJD (monitoring)
Considerations
- Severe liver disease may cause HA levels to be elevated (see liver disease below).
Available HA tests from VDI
- Osteoarthritis Panel
- Pre-Stem Cell Therapy Panel
- Osteoarthritis Assessment (wellness screening)
- Canine Complete Wellness
- Standalone HA Testing
Hyaluronic Acid: A DJD Biomarker
The Canine Joint
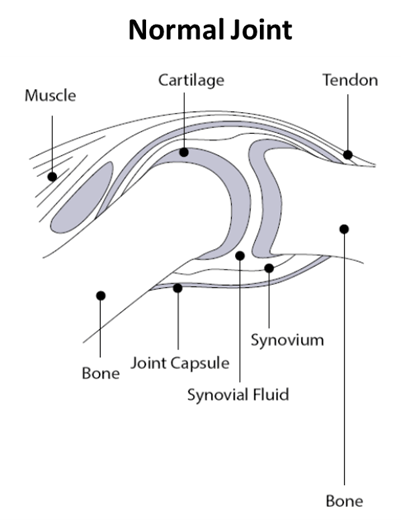
Synovial fluid: key to a healthy joint
Synovial fluid, found in the cavities of synovial joints, provides lubrication to reduce friction during movement. Within the joint are chondrocytes which are responsible for the extracellular matrix composition (ECM), regulation, and homeostasis. A key component of synovial fluid is hyaluronan, also known as hyaluronic acid (HA). HA has a unique capacity to bind and retain water molecules achieving excellent viscoelasticity. These properties make HA act as a lubricant and shock absorber, extremely useful in joints. Chondrocytes, cells within the articular cartridge, are responsible for the synthesis of synovial fluid including HA .
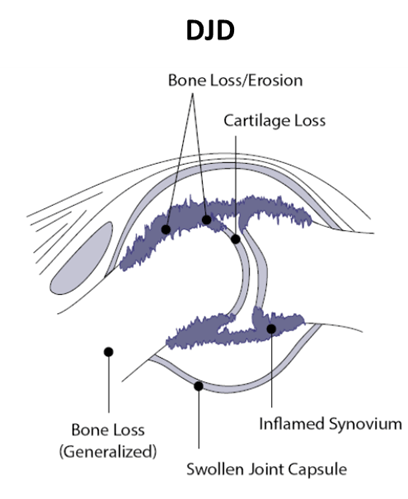
Degenerative Joint Disease
DJD is characterized by changes in the ECM, including bone loss, inflammation, and oxidative stress. The synovial membrane, which regulates the synovial fluid composition, develops synovitis. Loss of synovial fluid into the peripheral blood due to synovitis induces joint friction, more inflammation, pain, and stiffness. Over time, chondrocyte death and ECM loss form a vicious cycle with the progression of one aggravating the other.
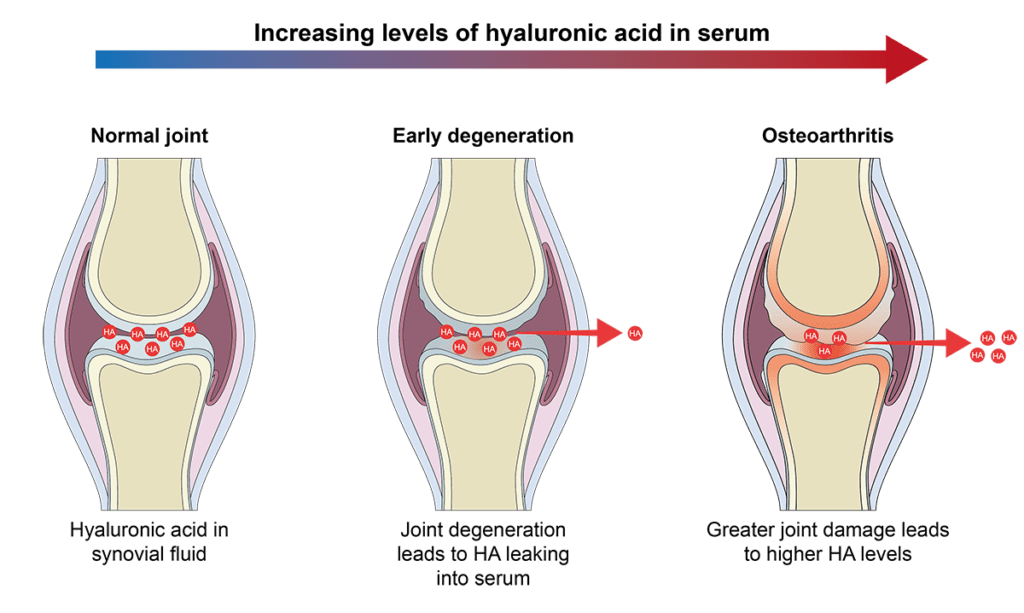
Hyaluronic Acid
The use of HA has been examined by a number of investigators in both human and veterinary medicine. The concept is simple: synovitis due to DJD allows HA to leak into the peripheral blood. HA has a very short half-life of 5 minutes therefore elevated serum HA (sHA) values correlate to the onset of DJD.
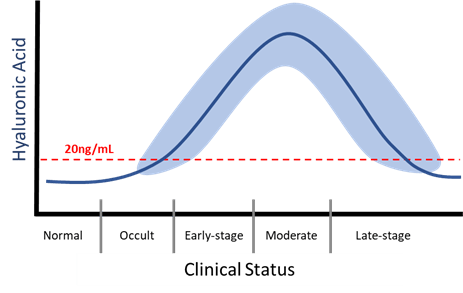
In the early to moderate stages of OA, serum concentration of HA increases as the chondrocytes continue to replace HA leaking out into the blood stream. Increasing concentration of HA correlates with disease severity. As disease worsens there is a decline in HA as chondrocytes have diminished capacity to produce HA, there is an increase in proteolytic enzymes destroying HA, and ultimately chondrocyte death in late-state disease. Depending upon treatment, HA level can increase again.
Inflammation in DJD
DJD is an inflammatory disease
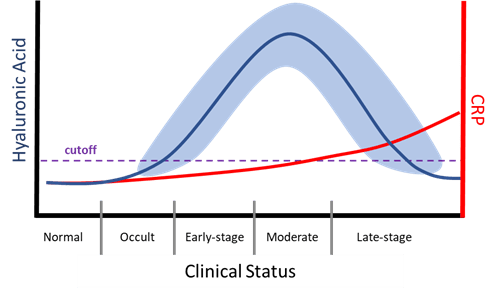
Osteoarthritis
Degenerative Joint Disease is ultimately is an inflammatory disease, however the initiation of which could be an injury or poor conformation. Most of the inflammation is localized at the joint and typically does not produce measurable levels of serum CRP or HPT until later; only IMPA will produce significant CRP/HPT due to its autoimmune nature. In OA, inflammation, and serum CRP/HPT, will progressively get worse as mechanical damage, bone loss, and chondrocyte death occurs. In an untreated patient, CRP/HPT will continually increase. With treatment, inflammation should be controlled and return to normal.
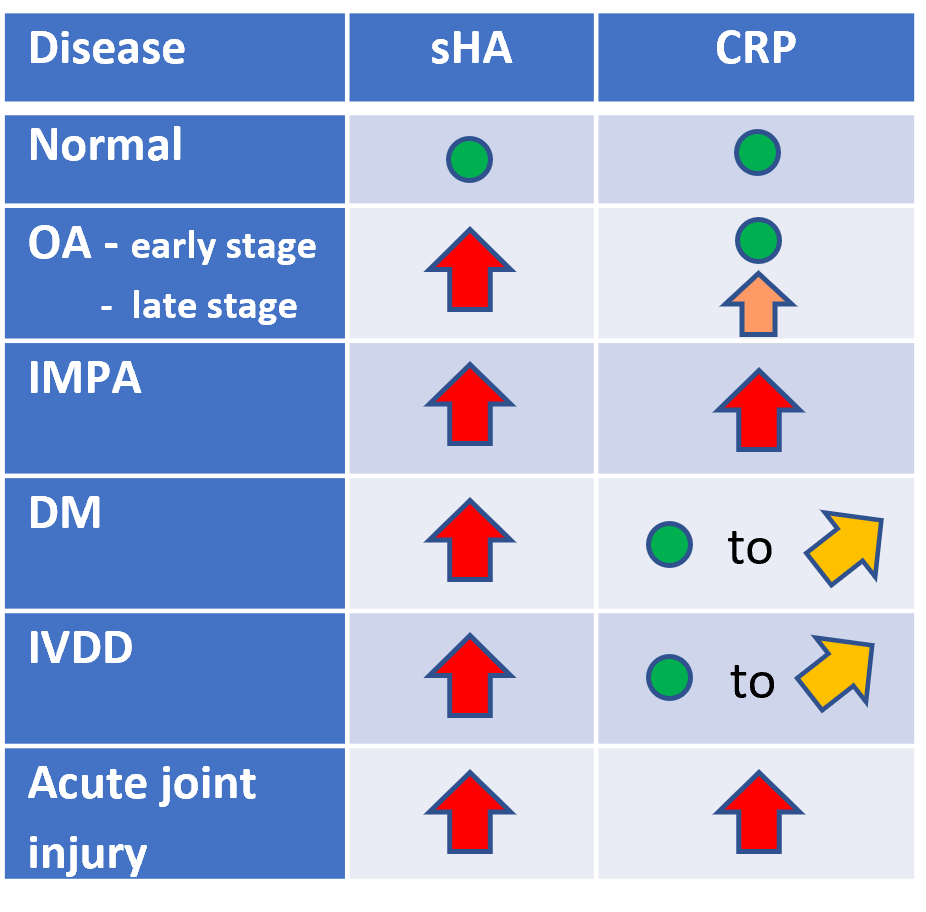
Immune-Mediated Polyarthritis (IMPA)
IMPA significantly differs from other OA in its autoimmune origin. It is classified based upon whether it is erosive or non-erosive. IMPA is believed to be a result of immune-complex deposition within the synovium resulting in a sterile synovitis. The antigenic stimuli can be from a wide range or sources such as a distant infection, neoplasia, drug reaction, and others. This antigenic stimulation of the immune system triggers a moderate to strong inflammatory response resulting in elevated concentrations of CRP/HPT at disease onset.
Degenerative Myelopathy (DM)
DM is necrosis within the spinal cord segments with secondary demyelination. DM presents as a slowly progressive, non-painful myelopathy that will over time progress cranially . DM will present with elevated HA and normal to mildly elevated CRP/HPT.
Intervertebral Disk Disease (IVDD)
IVDD is clinically similar to DM and the differential diagnosis can be difficult. Both result in degeneration of the spinal cord. IVDD is believed to be a reduction of nutrients to the spinal cord causing chondrocyte death and changes in the ECM. There is no known cure for IVDD. IVDD will present with elevated HA and normal to mildly elevated CRP.
Hyaluronic Acid in DJD Therapy
Treatment and Therapy

There is no cure for OA, the goal of therapy is to help alleviate joint pain, to reduce inflammation and delay disease progression, and to restore joints to normal function with an overall increase in the quality of life. Hyaluronic Acid can be used in conjunction with a number of therapies to monitor therapy effectiveness.
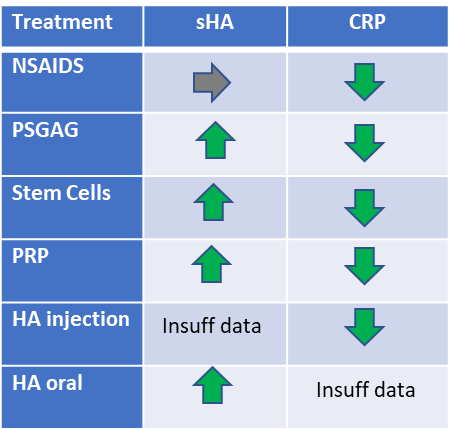
NSAIDS
NSAIDS are used to control inflammation and to provide patient comfort. When used early and consistently studies show disease progression is slowed and overall quality of life is increased. NSAIDS do not stimulate the production of hyaluronic acid.
PSGAGs
Polysulfated glycosaminoglycan (PSGAG) is an intramuscular injection for the control of signs associated with non-infectious degenerative and/or traumatic arthritis of synovial joints. While the exact mechanism of action is unknown, PSGAG is known to inhibit proteolytic enzymes which includes hyaluronidases. VDI’s own internal data shows that patients treated with PSGAG have increasing concentrations of sHA.
Stem Cells/PRP
Mesenchymal stem cell (MSC) therapy or platelet rich plasma (PRP) are becoming more common when NSAIDS fail to provide the relief needed. MSC therapy is focused on their anti-inflammatory, immunomodulatory, and immunosuppressive potential. While the exact mechanism of action is still being investigated, in-vitro studies show stem cells can differentiate toward chondrocytes . With successful treatment the concentration of sHA is increased.
PRP is rich in platelet-derived growth factors. The logic behind PRP is a supra-physiological amount of growth factors delivered directly at the site of the damaged joint. The goal is to promote natural healing and tissue regeneration. Studies mostly focus on its ability to heal fractures. Use in OA has limited data however in one study use of PRGR did increase sHA concentration, indicating a stimulating effect on the chondrocytes .
Hyaluronan –Injection and Oral
Injection
Intra-articular injection of HA (IA-HA) is an established procedure in both human and veterinary medicine. IA-HA improves shock absorption, joint lubrication, anti-inflammatory effects, chondroprotection, and improvements to the ECM. Studies show improvement in lameness within 1 week and for up to 6 months post injection. Combined therapy with corticosteroids shows additional benefit although the use of corticosteroids long term has significant disadvantages.
Oral
HA, a disaccharide polymer, ranges in length from 5 kDa to 20,000 kDa. Isotopic tracer studies show intestinal absorption of 80% when a mid-sized molecular weight (MW) is used. In fact, the MW weight of oral HA is critical for the effective treatment of OA. Very high MW HA (>2,000 kDa) is too large to be absorbed well by the intestinal barrier and low MW HA can be pro-inflammatory (1).
In a study looking at radioactively labeled 1,000 kDa oral HA in rats, scans showed significant uptake within the joints of 100-300 times greater than the control group (2). To evaluate if oral HA supplementation is effective in stimulating the production of HA and the reduction of inflammatory markers, a cohort of 55 dogs undergoing CCL surgery were divided into two groups for a prospective, randomized, double-blinded, clinical study (3). One group was provided 800-1000 kDa HA, and the other a placebo. Over a ten week recovery synovial fluid was examined for HA and other biomarkers.
In dogs supplemented with oral HA, synovial fluid HA concentration significantly increased whereas the placebo group declined. Additionally, pro-inflammatory marker paraoxonase-1 significantly declined in the HA group. The authors stated, “results demonstrated that postoperative oral administration of HMW-HA in canine patients with OA secondary to CCL injury leads to improvements in OA biomarkers measured in synovial fluid, specifically in HA and PON-1 concentrations”.
- Gupta RC, Lall R, Srivastava A, Sinha A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front Vet Sci. 2019 Jun 25;6:192. doi: 10.3389/fvets.2019.00192. PMID: 31294035; PMCID: PMC6603175.
- Da Riz F, Higgs P, Balogh L, Polyak A, Mathe D, Kiraly R, Thuroczy J, Terez M, Janoki G, Ting Y, Bucci LR, Schauss AG. Absorption, uptake and tissue affinity of high-molecular-weight hyaluronan after oral administration in rats and dogs. J Agric Food Chem. 2008 Nov 26;56(22):10582-93. doi: 10.1021/jf8017029. PMID: 18959406.
- Serra Aguado CI, Ramos-Plá JJ, Soler C, Segarra S, Moratalla V, Redondo JI. Effects of Oral Hyaluronic Acid Administration in Dogs Following Tibial Tuberosity Advancement Surgery for Cranial Cruciate Ligament Injury. Animals (Basel). 2021 Apr 27;11(5):1264. doi: 10.3390/ani11051264. PMID: 33925642; PMCID: PMC8146498.
Liver Disease & HA

HA is widely present in the body’s ECM. The liver rapidly destroys circulating HA; the half-life of HA is less than 5 minutes. In severe liver disease, the destruction of HA is delayed resulting in higher sHA values. Patients with severe liver disease may present with high levels of sHA and not have DJD.
The type of liver disease that will increase sHA is limited to chronic hepatitis and chronic cirrhosis that produces liver fibrosis as well as patients with congenital portosystemic shunt. In these patients, hepatic fibrosis in response to an acute or chronic liver injury to parenchymal cells curtails the degradation of HA raising sHA levels. In situations where performing a liver biopsy is not possible, studies show sHA level to be a reliable indicator of hepatic fibrosis with a sensitivity of 82% and specificity of 89% .
