Determining the root cause of hypo or hypercalcemia should be quick. Using additional biomarkers like PTH and Vitamin D, we can quickly determine what may be play, whether it’s hypercalcemia of malignancy, hyperparathyroidism, or hypoparathyroidism. Explore some common findings below for each of these situations, and utilize the VDI Calcemia Panel to expedite your differential.
Sections:
- Secondary Hyperparathyroidism (with normocalcemia)
- Masked Primary Hyperparathyroidism
- Hypercalcemia of Malignancy
- Bonus Application: Vitamin D Toxicity
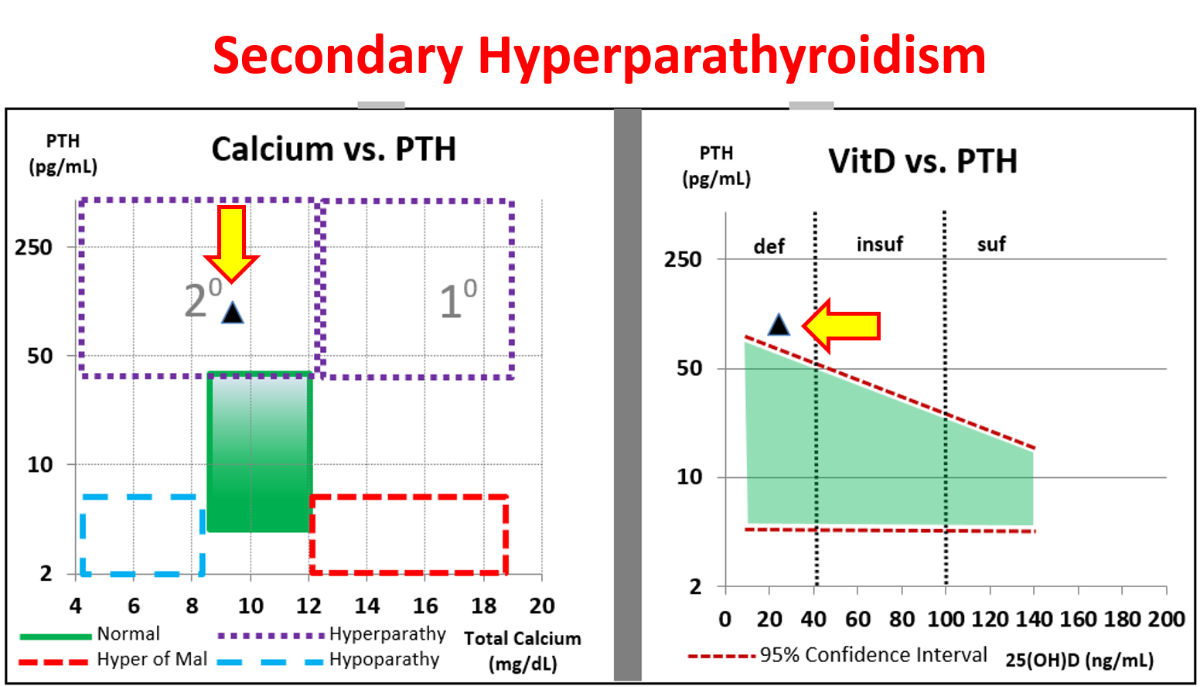
1. Secondary Hyperparathyroidism
Can you have Secondary hyperparathyroidism with normal calcium? Yes!
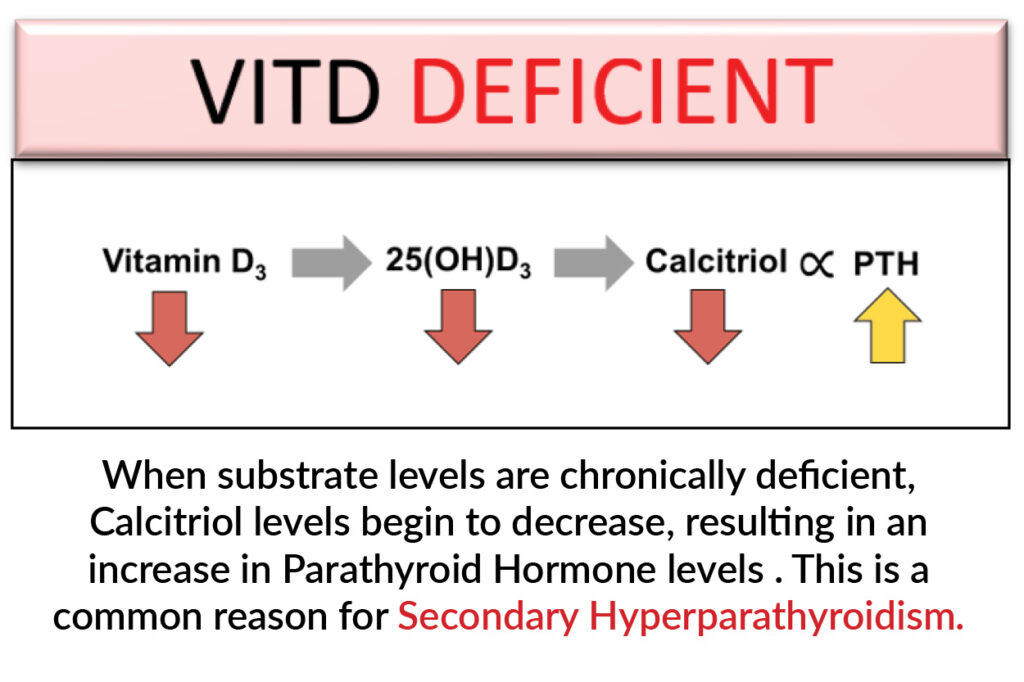
Secondary hyperparathyroidism reflects PTH-independent normo/hypocalcemia. In simple terms, a calcium level that is not being driven by PTH but rather secondary to other reasons. The most common reason is vitamin D deficiency.
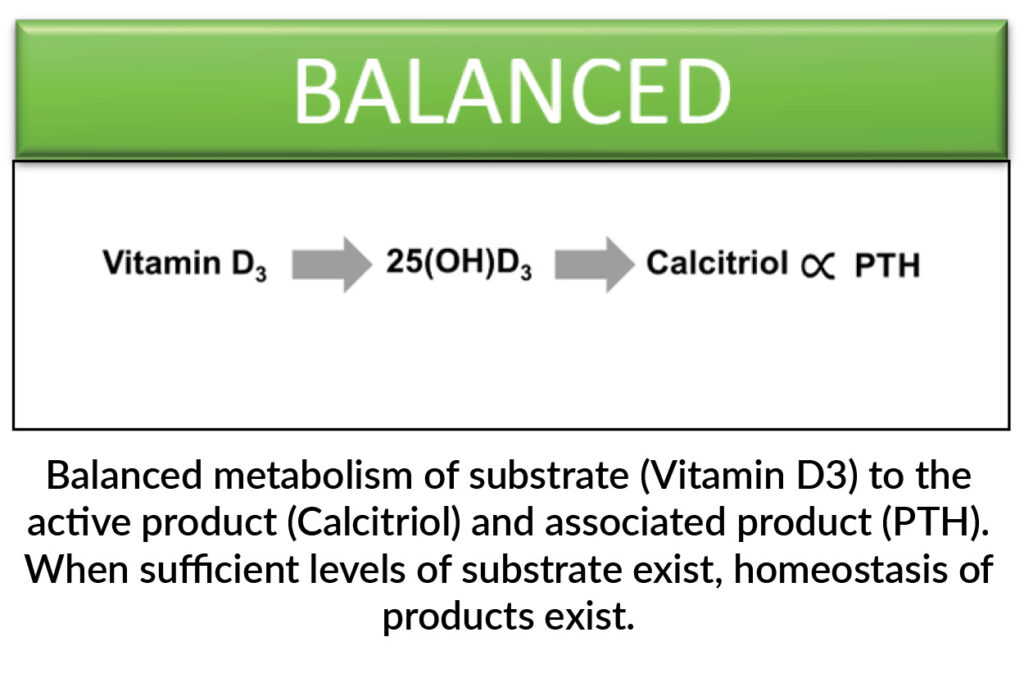
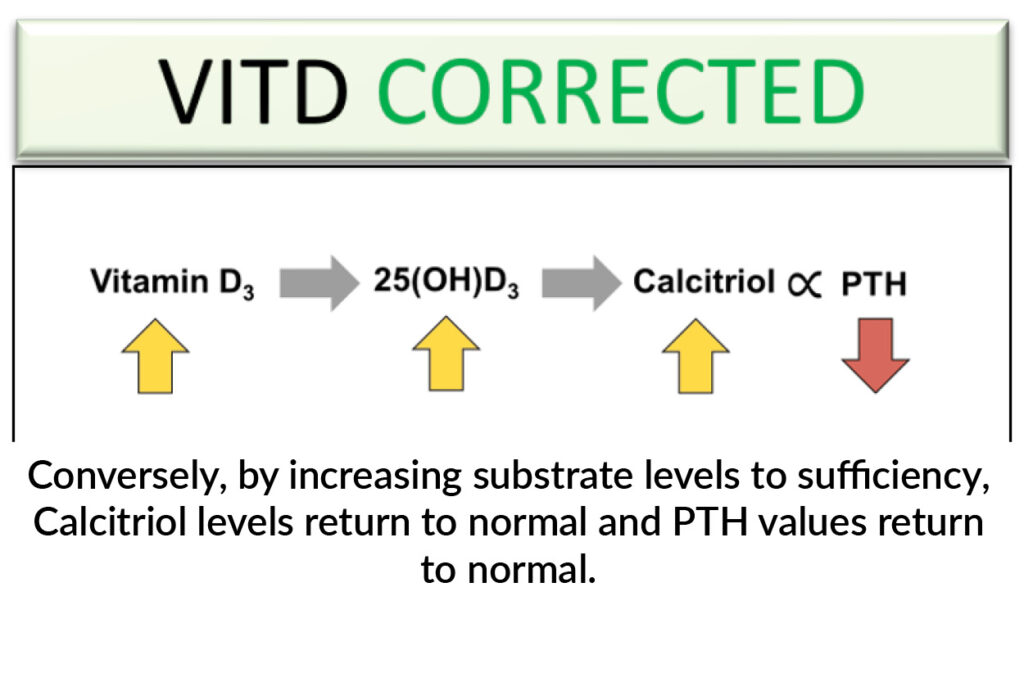
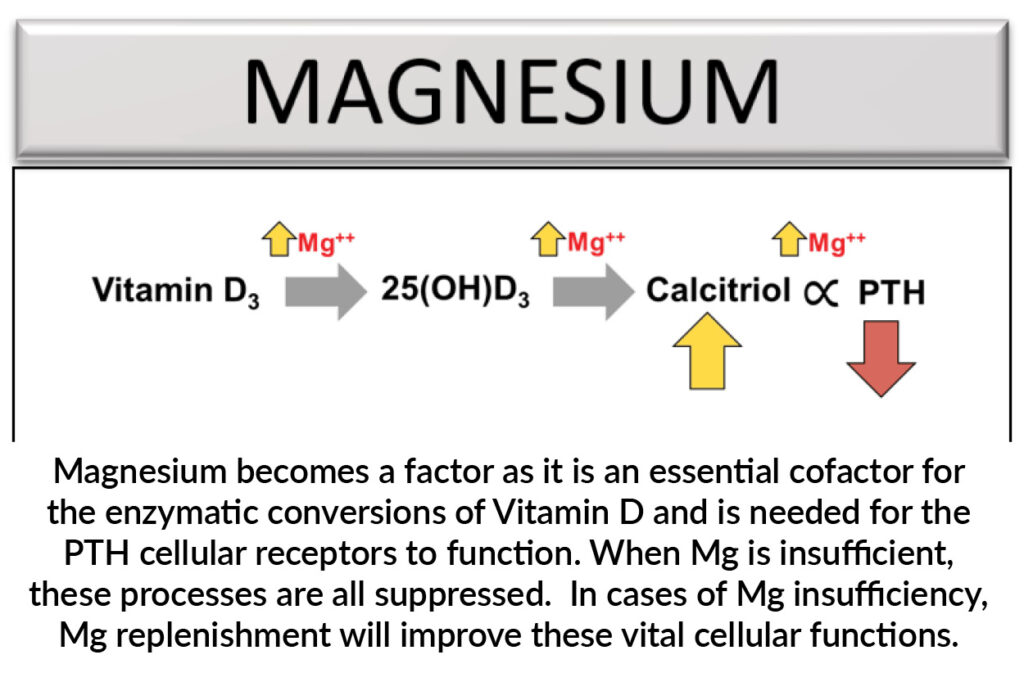
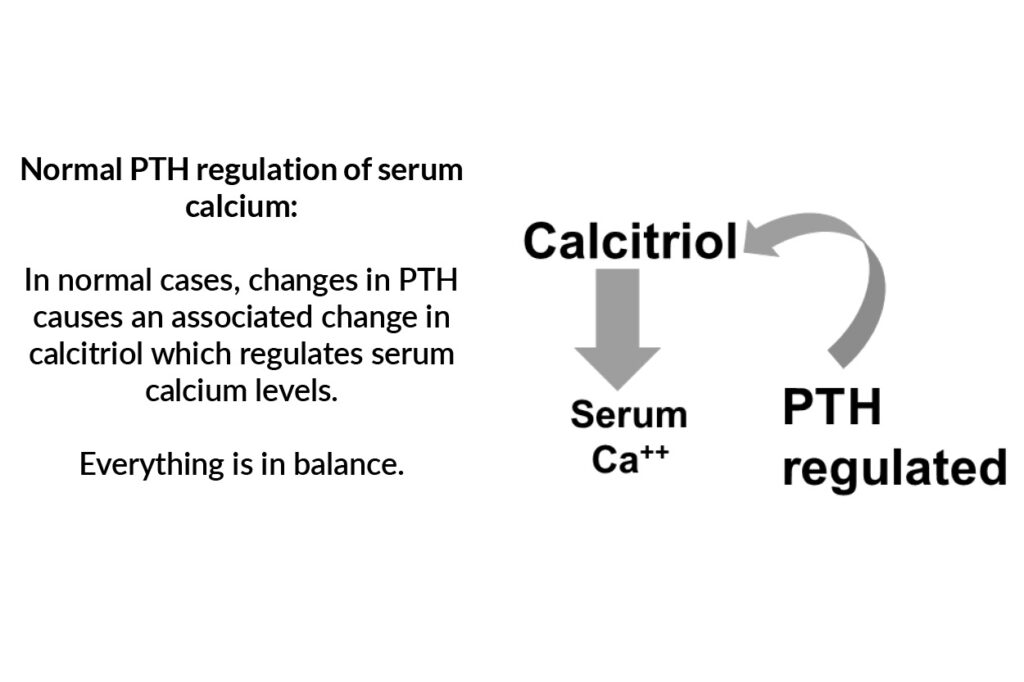
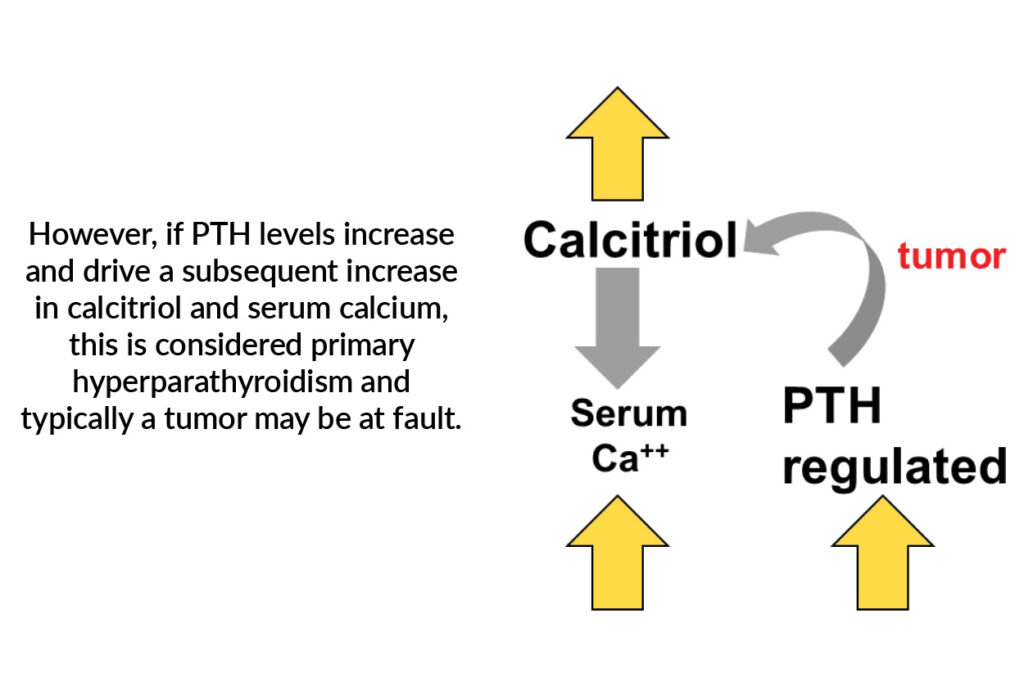
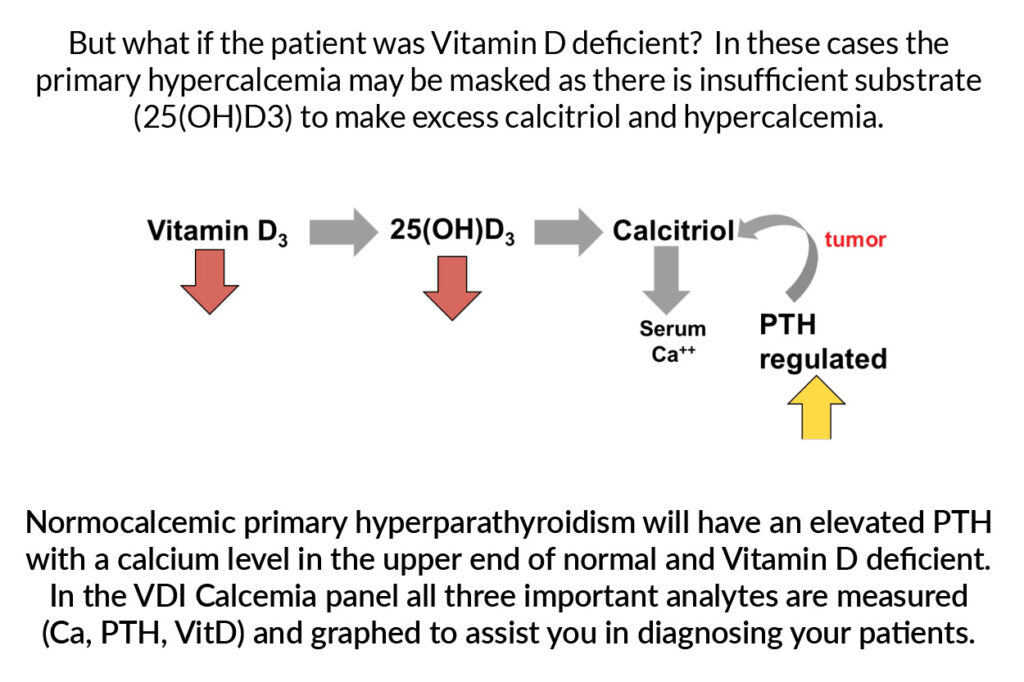
When we talk about Vitamin D it generally covers three different forms, Vitamin D3, 25(OH)D3, and calcitriol; the latter being responsible for serum calcium level. These conversions are all enzymatic – the more or less substrate you have; the more or less product you have. Scroll through the slides below to see this in action.
Secondary hyperparathyroidism may be found in:
– Vitamin D deficiency
– Renal patients
– Low or low-normal calcium
– Senior dogs and cats
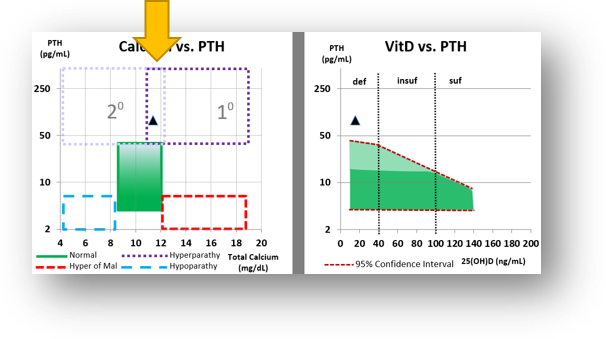
VDI Calcemia Panel Graph:
Secondary Hyperparathyroidism zone can be found in the top left – elevated PTH with low or low-normal calcium. Be sure to reference the PTH vs VitD chart to see how Vitamin D levels may be contributing.
2. Masked Primary Hyperparathyroidism
Is it possible to have a primary hyperparathyroidism with normal calcium? Also Yes!
Unlike in secondary hyperparathyroidism, primary hyperparathyroidism is PTH-dependent, meaning calcium levels are being driven by high levels of parathyroid hormone. Then why is calcium normal?
Masked primary hyperparathyroidism may be found in:
– Vitamin D deficiency
– High-normal calcium
– Senior dogs and cats
VDI Calcemia Panel Graph:
The overlap of Primary and Secondary Hyperparathyroidism zones, with high-normal calcium is where a “masked” primary hyperparathyroidism may be found.
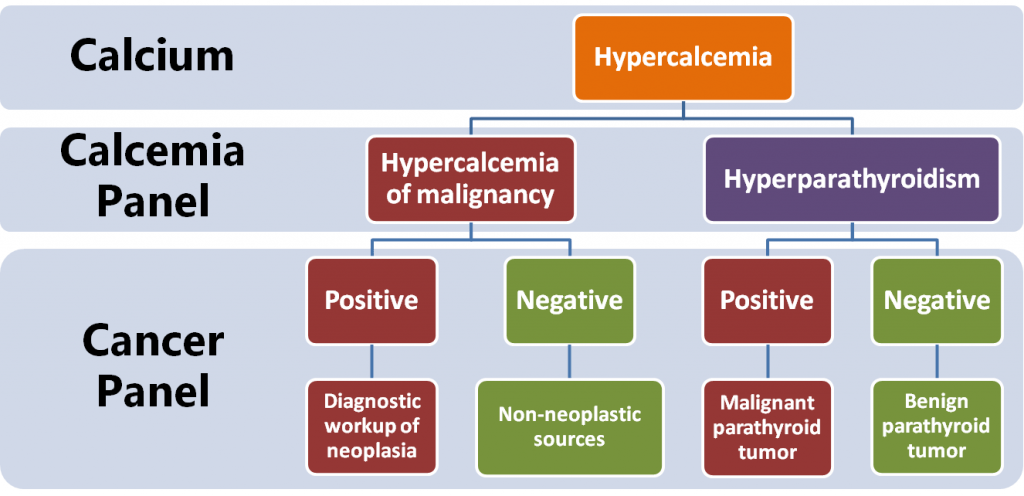
3. Hypercalcemia of Malignancy
The term “hypercalcemia of malignancy” is routinely used when calcium is elevated and PTH is below normal, and for good reason— this situation is often a result of malignant neoplasia, particularly lymphoma, anal sac adenocarcinoma, or multiple myeloma. However, many other diseases can fall into this category such as granulomatous disease, hyperthyroidism, vitamin D intoxication, and Addison’s disease.
When a patient presents with hypercalcemia of unknown origin, a good place to begin is with a calcium and PTH measurement. If hypercalcemia of malignancy is present, the VDI Calcemia Panel report will plot within the lower red zone:
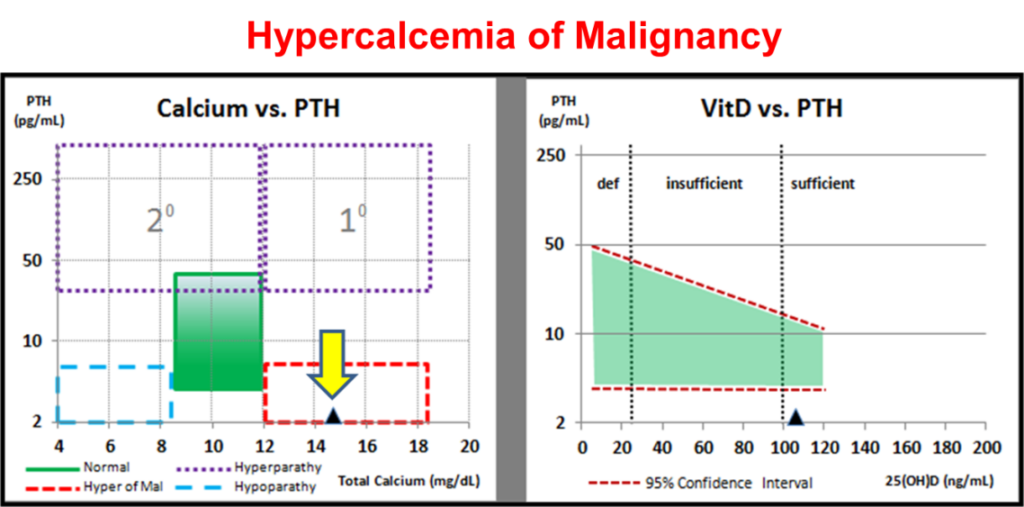
To rule in/out neoplasia as the reason for hypercalcemia, reflexing to the VDI Cancer Panel will provide fast insight if neoplasia is suspect. If negative, other non-neoplastic causes can be further investigated.
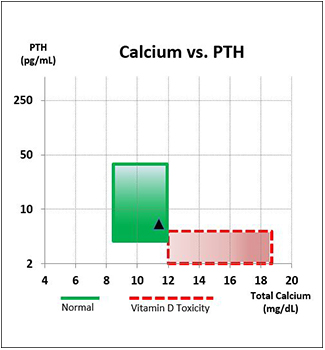
4. Bonus Application: Vitamin D Toxicity
A special application of the Calcemia Panel is the Vitamin D Toxicity Panel. As mentioned in section 3, one cause of “hypercalcemia of malignancy” could be Vitamin D Toxicity. More commonly, however is concern over excess Vitamin D intake, and the question becomes: Is the pet experiencing toxicosis? For that we evaluate the same 3 markers: PTH, Calcium, and Vitamin D.
To know if a patient has suffered vitamin D intoxication three questions need to be answered:
1. Has the parathyroid gland responded appropriately and shut down production of PTH?
2. Does the patient have hypercalcemia?
3. Does the patient have abnormally high levels of 25(OH)D?
For a patient to have vitamin D intoxication, all three questions need to be answered “YES”.
Calcium vs PTH
To answer questions 1 and 2, the panel plots Ca vs PTH, with quick visual representation of where Vitamin D Toxicity occurs
When the marker falls within the green zone, even with elevated vitamin D, the patient is not Vitamin D Toxic. When the marker falls into the red zone, likelihood of toxicity is much higher.
Vitamin D stores (25OHD)
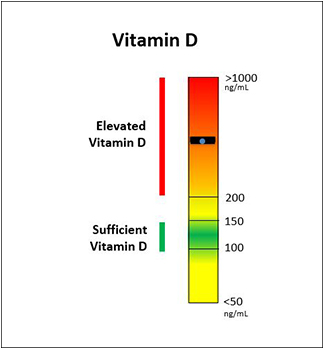
Sufficient range for Vitamin D is 100-150 ng/mL in dogs and cats. Panel reports 50-1000 ng/mL.
Elevated Vitamin D levels should be corrected. In absence of toxicity from the first chart, elevated Vitamin D should not be overly concerning unless patient is not managed (see TIME section below)
Vitamin D: 25(OH)D
Approximately 75% of unsupplemented dogs and cats are vitamin D insufficient (1). The primary source of vitamin D is through dietary protein (chicken, lamb, fish, etc) and a minor amount via food supplementation (AAFCO guidelines 500 IU D3/kg dry food (2)). In vitamin D intoxication, excess supplement is the culprit. Patients with vitamin D intoxication should exhibit abnormal levels of 25(OH)D.
- Selting K (2015) The effect of diet on serum 25-hydroxyvitamin D concentrations in dogs. BMC Res Notes
- AAFCO (2014) AAFCO methods for substantiating nutritional adequacy of dog and cat foods
PTH
In the event of excess calcitriol production in vitamin D intoxication, PTH production should shut down completely. In some patients with subclinical primary hyperparathyroidism, vitamin D deficiency can mask this condition. When the patient consumes food with more vitamin D, even though vitamin D levels may not be abnormal, the parathyroid gland fails to shut down yielding hypercalcemia.
Calcium
The final event in vitamin D intoxication is hypercalcemia. Patients with vitamin D intoxication should exhibit hypercalcemia.
Time
The Vitamin D Toxicity Panel represents a moment in time- a the blood draw. Even if the patient is not presently Vitamin D toxic, these values can change over time, especially if the source of Vitamin D excess is not removed. It’s important to monitor the patient and retest until Vitamin D levels drop below 200ng/mL and PTH and Calcium levels return to – or remain – normal.